Orthodontics is a specialized branch of dentistry focused on the diagnosis, prevention, and treatment of dental and facial irregularities. Patient assessment is a crucial step in orthodontic treatment planning, as it allows orthodontists to determine the appropriate course of action tailored to each patient’s needs. In this article, we will delve into the process of patient assessment in orthodontics, including recognizing who needs orthodontic treatment, the hierarchy of patient assessment, and the various aspects of extra-oral and intra-oral examinations. (1)
Recognizing Who Needs Orthodontics
Orthodontic treatment is recommended for individuals with various dental and facial irregularities, which may include:
- Malocclusion: Malocclusion refers to improper alignment of the teeth when the jaws are closed, leading to issues such as overcrowding, overbites, underbites, crossbites, and open.

- Crowded Teeth: Crowding occurs when there is insufficient space in the dental arch for all the teeth to align properly, leading to overlapping or crooked teeth.
- Misaligned Jaws: Misalignment of the upper and lower jaws can result in functional problems such as difficulty chewing or speaking, as well as aesthetic concerns.

- Protruding Teeth: Protruding or “buck” teeth can impact facial aesthetics and increase the risk of dental trauma.

- Dental Asymmetry: Asymmetry in the positioning of teeth or jaws can affect facial symmetry and overall appearance. (2)
Patient Assessment Hierarchy in Orthodontics
The patient assessment process in orthodontics follows a structured hierarchy to ensure comprehensive evaluation and accurate diagnosis. This hierarchy typically includes the following steps:
- Medical and Dental History: Gathering information about the patient’s medical history, including any previous dental treatments or surgeries, allergies, medications, and systemic conditions that may impact orthodontic treatment.
- Clinical Examination: Conduct a thorough examination of the patient’s facial structure, dental alignment, and occlusion (how the teeth fit together).
- Radiographic Evaluation: Utilizing various imaging techniques such as X-rays, panoramic radiographs, and cephalometric radiographs to assess dental and skeletal structures in detail.
- Photographic Analysis: Taking intraoral and extraoral photographs to document the patient’s facial and dental appearance from different angles, providing valuable visual aids for treatment planning and monitoring progress.
- Dental Models: Creating plaster or digital models of the patient’s teeth to evaluate their alignment and occlusion more precisely. (3)
Extra-oral assessment
Extra-oral assessment in orthodontics involves evaluating facial structures, soft tissues, and overall facial symmetry to gather essential information for diagnosis and treatment planning. This assessment provides valuable insights into the patient’s facial aesthetics, growth patterns, and functional aspects. Let’s delve into the details of extra-oral assessment:
1. Facial Symmetry:
- Observation of the face from the front to assess the symmetry of the eyes, ears, nose, and
- Any asymmetry in facial features may indicate underlying skeletal or soft tissue
- Assessing facial symmetry helps in identifying potential sources of aesthetic concerns and guiding treatment decisions.

2. Profile Analysis:
- Evaluation of the profile view to assess the relationship between the forehead, nose, lips, and chin.
- Analysis of the profile helps in identifying any discrepancies such as a retruded or protruded upper or lower jaw, lip incompetence, or a prominent chin.
- Understanding the profile aids in planning orthodontic treatment to achieve facial harmony and balance.
3. Soft Tissue Examination:
- Assessment of the lips, cheeks, and chin for any abnormalities or
- Examination of soft tissues helps in detecting issues such as lip incompetence, excessive gingival display (gummy smile), or tension in the facial muscles.
- Soft tissue evaluation is crucial for achieving favorable treatment outcomes and facial.

4. Functional Evaluation:
- Observation of the patient’s jaw movements, including opening, closing, and lateral
- Assessment of functional movements helps in identifying any functional issues such as temporomandibular joint (TMJ) disorders, muscle imbalances, or habitual behaviors.
- Functional evaluation guides treatment planning to address functional discrepancies and improve overall jaw function.
5. Growth Assessment:
- Estimation of the patient’s growth pattern and stage of
- Evaluation of growth helps in anticipating future orthodontic needs and determining the optimal timing for treatment interventions.
- Monitoring growth patterns enables orthodontists to plan treatments that take into account the patient’s growth potential and achieve stable long-term results.
6. Photographic Documentation:
- Taking standardized extra-oral photographs from different angles, including frontal, lateral, and oblique views.
- Photographic documentation serves as a valuable tool for treatment planning, communication with patients, and monitoring treatment progress.
- Photographs provide visual references for assessing facial changes throughout the treatment process and comparing pre- and post-treatment outcomes.
7. Radiographic Evaluation:
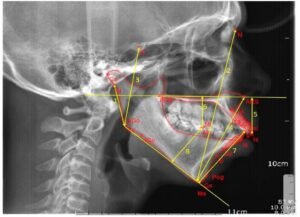
- Utilizing cephalometric radiographs and other imaging techniques to assess skeletal structures and facial proportions.
- Radiographic evaluation complements clinical examination by providing detailed information about craniofacial morphology, dental development, and airway anatomy.
- Radiographs aid in diagnosing skeletal discrepancies, evaluating tooth eruption patterns, and planning orthodontic treatment strategies. (4,5)
Skeletal/Dental Relationship Assessment
Assessing the skeletal and dental relationship is essential for diagnosing malocclusions and planning appropriate treatment. This assessment involves:
- Cephalometric Analysis: Analyzing cephalometric radiographs to evaluate the skeletal relationships between the jaws, teeth, and cranial base.
- Dental Cast Analysis: Examining dental models to assess tooth size, shape, and alignment, as well as the relationship between the upper and lower teeth.
- Bite Analysis: Evaluating the patient’s bite to determine the presence of overbites, underbites, crossbites, or open bites, which indicate malocclusion.

- Functional Examination: Assessing how the teeth come together during chewing and speaking to identify any discrepancies in the occlusal relationship.
- Orthodontic Indices: Using standardized indices such as the Index of Orthodontic Treatment Need (IOTN) to quantify the severity of malocclusion and prioritize treatment. (6,7)
Malocclusion Classification and Clinical Features
Malocclusion refers to misalignments of the teeth or improper relation between the dental arches, which can lead to functional issues and aesthetic concerns. These malocclusions are classified into different categories based on their skeletal and dental components. Each classification has distinct clinical features, which aid in diagnosis and treatment planning. Let’s explore the classification and clinical features of common malocclusions:
1. Class I Malocclusion:
Clinical Features:
- Class I malocclusion is characterized by a normal skeletal relationship between the upper and lower jaws.
- The teeth may be misaligned within the dental arches, presenting with issues such as crowding, spacing, or rotations.
- Dental midlines usually align with the midline of the
- There may be normal overbite (vertical overlap of the upper teeth over the lower teeth) and overjet (horizontal projection of upper teeth over lower teeth).
2. Class II Malocclusion:
Clinical Features:
- Class II malocclusion is identified by the protrusion of the upper jaw relative to the lower jaw, leading to an overbite.
- The upper front teeth (maxillary incisors) protrude significantly beyond the lower front teeth (mandibular incisors).
- The lower jaw may appear retruded in relation to the upper
- Class II malocclusion can be further categorized into Class II Division 1 and Class II Division 2, depending on the severity of overbite and the position of the lower incisors relative to the upper incisors.
3. Class III Malocclusion:
Clinical Features:
- Class III malocclusion is characterized by the protrusion of the lower jaw relative to the upper jaw, leading to an underbite.
- The lower front teeth (mandibular incisors) are positioned anteriorly in relation to the upper front teeth (maxillary incisors).
- The upper jaw may appear retruded or the lower jaw may appear
- Class III malocclusion can present with dental crowding or spacing similar to Class I malocclusion. (8)

4. Open Bite:
Clinical Features:
- An open bite occurs when there is no vertical overlap between the upper and lower front
- The molars may be in normal occlusion, but there is a lack of contact between the incisors when the jaws are closed.
- Open bites can be caused by habits like thumb sucking or tongue thrusting, or skeletal discrepancies between the upper and lower jaws.
- Patients with open bites may experience difficulties in biting and chewing certain
5. Crossbite:
Clinical Features:
- Crossbite refers to a lateral misalignment of the upper and lower teeth, where some of the upper teeth sit inside the lower teeth when the jaws are closed.
- Crossbites can occur in the front teeth (anterior crossbite) or the back teeth (posterior crossbite).
- Anterior crossbites may lead to abnormal wear of the incisors and affect facial
- Posterior crossbites can cause functional issues such as interference in chewing and speaking. (9,10)

In summary, understanding the classification and clinical features of malocclusions is essential for orthodontic diagnosis and treatment planning. By identifying the specific type of malocclusion and its associated features, orthodontists can develop personalized treatment approaches to address functional concerns and improve the patient’s overall oral health and aesthetics.